SENSORINEURAL TINNITUS
Sensorineural tinnitus develops when the sensory or neurological system causes tinnitus. This initiation could occur in the cochlea, auditory nerve, temporal lobe, or other regions of the nervous system across the brain. The most frequent type of tinnitus, sensorineural tinnitus, is almost invariably associated with sensorineural hearing loss. Tinnitus can be caused by even little variations in hearing thresholds. It is vital to remember that human hearing may reach up to 20 kHz, whereas hearing is normally tested up to 8 kHz. Patients with tinnitus may have adequate audiometric thresholds but have difficulties hearing sounds when there is background noise.
Presbycusis Tinnitus
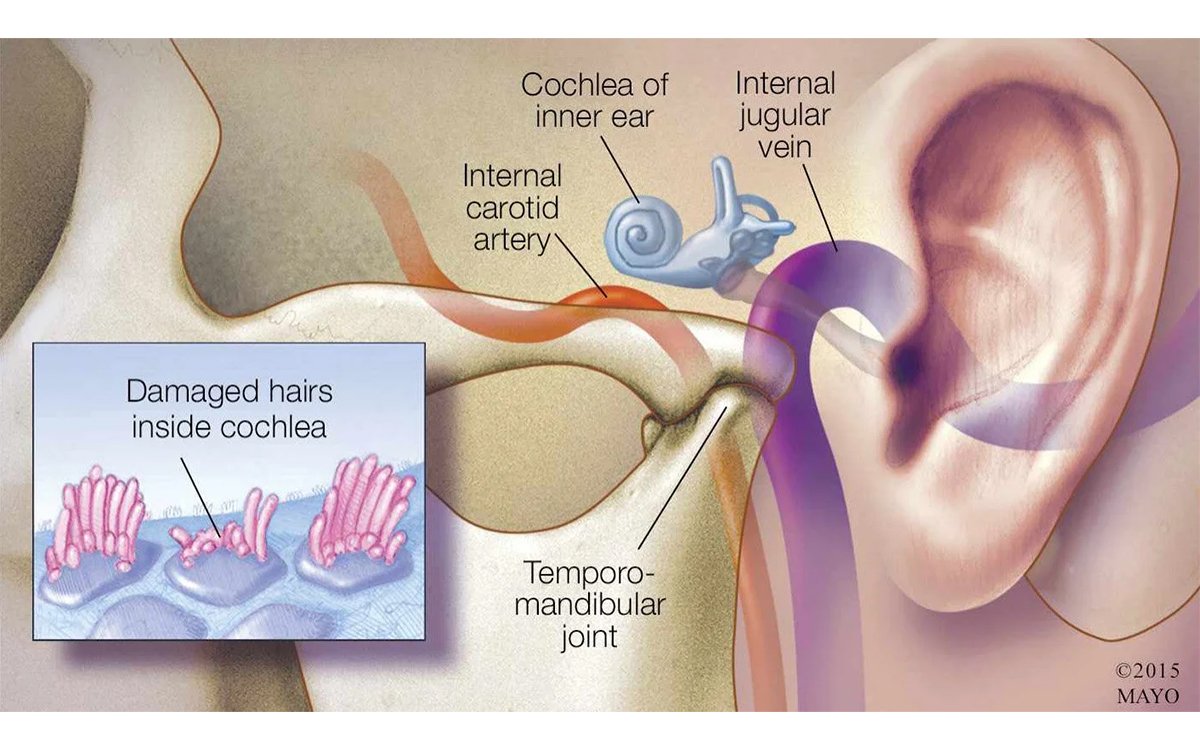
As people age, they gradually lose their hearing. Age-related hearing loss (presbycusis) is the leading communication issue and one of the top three chronic health conditions among the elderly. It impairs the ability to understand communication, resulting in social isolation. Some people may also experience tinnitus as a result of the natural aging process, which can be difficult to separate from other unknown reasons. To establish presbycusis tinnitus, there must be an insidious onset of a high-frequency sensorineural hearing loss, usually bilateral and symmetric, that occurs after a certain age (e.g., 60 years or even 70 years), and a progression of loss over time, with no other likely causes. Hearing alterations with aging are linked to damage to the cochlear sensory hair cells.
Metabolic Tinnitus
To function properly, the auditory system requires glucose and a lot of energy. The supply of oxygen and glucose is critical for maintaining inner ear fluid balance. Changes in blood flow or metabolites impede inner ear function, harming the auditory system and potentially triggering hearing impairments such as tinnitus. This article discusses some clinical circumstances that may impact inner ear homeostasis.
Diabetes type II:Hyperglycemia can affect the cochlea. Abnormal blood glucose levels, even over short periods of time, can cause subclinical pathologic changes such as cochlear damage and auditory neuropathy, as well as hearing loss and tinnitus. Diabetics’ hearing evaluations reveal low-frequency hearing loss, which may or may not be coupled with mid-frequency and high-frequency hearing loss and is more evident in the right ear.
Hypothyroidism:Hypothyroidism, a frequent endocrinological condition, is caused by diminished thyroid hormone action in peripheral tissues, which slows down overall body functioning. The likelihood of having hypothyroidism increases with age, and it is ten times more common in women than males. Hypothyroidism’s decreased cerebral blood flow and glucose metabolism may induce cochlear damage, hearing loss, and tinnitus. Hearing loss is often bilateral and mild to moderate, with a flat audiogram.
Dyslipidemia:Hypothyroidism, a frequent endocrinological condition, is caused by diminished thyroid hormone action in peripheral tissues, which slows down overall body functioning. The likelihood of having hypothyroidism increases with age, and it is ten times more common in women than males. Hypothyroidism’s decreased cerebral blood flow and glucose metabolism may induce cochlear damage, hearing loss, and tinnitus. Hearing loss is often bilateral and mild to moderate, with a flat audiogram.
Anemia:Anemia (low hemoglobin levels) affects the cochlea by reducing oxygen delivery, resulting in sensorineural hearing loss and tinnitus.
Vitamin and mineral deficiencies:Several studies have connected vitamin and mineral deficits with hearing loss and tinnitus, including vitamin B12, B1, D3, zinc, and magnesium.
Noise-Induced Tinnitus Noise
Exposure is one of the leading causes of tinnitus. Noise-induced hearing loss (NIHL) is characterized by a notched audiogram, poor hearing at 3 to 6 kHz, and then improvement at 8 kHz, for example. Subgrouping noise-induced tinnitus may necessitate a history of noise exposure. It may also be beneficial to distinguish between numerous years of noise exposure and a rapid NIHL, maybe caused by an impulse noise, such as a gunshot. Airbag explosions can cause impulsive noise-induced tinnitus, but they may also cause head trauma, which must be removed from the subgrouping. If the noise-induced tinnitus affected only one ear, such an approach would provide for significant within-subject control. Furthermore, with sudden-onset noise-induced tinnitus (for example, after an explosion or gunshot), acute tinnitus effects can be distinguished from long-term noise impacts, which can affect numerous sections of the nervous system.
Noise-induced hearing loss:NIHL is often caused by prolonged, continuous noise exposure. The level of inner ear damage is determined by the intensity of the sound, the time of exposure, and hereditary predisposition. Tinnitus is typically bilateral, continuous, and high in pitch.
Acoustic trauma:Acoustic Trauma. Hearing loss is caused by a single or repeated exposure to sudden, intense noise, such as firearm shooting, car airbag release, and recreational music. It has been reported to immediately cause tinnitus.
Acoustic shock:Acoustic shock injury (ASI) is caused by a brief exposure to rapid, unexpected loud sounds, which can cause tinnitus, ear pain, ear pressure, hyperacusis/phonophobia, and vertigo. Insomnia, headaches, and disorientation are some of the nonotological symptoms. There may be high levels of emotional trauma and anxiety. Typically, symptoms are transient and diminish within hours to days of exposure. ASI has largely been described by contact center employees who use a telephone headset or handset. Clinical examinations and audiometric tests are often normal. The postulated neurophysiologic process involves an increased startle reaction and contraction of the tensor tympani muscle.
Sudden Sensorial Hearing Loss and Tinnitus
Sudden sensorineural hearing loss (SSHL) is defined as a hearing loss of 30 decibels or more in three consecutive frequencies in one or both ears within 72 hours. Tinnitus linked with SSHL is usually unilateral and has a sudden onset. As a comorbidity, it may worsen and become the patient’s primary concern. Possible causes include viral inflammation, vascular blockage, and immunological disorders, all of which can harm the inner ear, cochlea, or auditory pathways. Some causes of SSHL require immediate diagnosis, such as vestibular schwannoma (acoustic neuroma), stroke, malignancy, noise, and ototoxic medicine. Although tinnitus elicits stronger emotional responses in these people, it is a good outcome factor for hearing recovery.
Rapidly Progressive Bilateral Sensorineural Hearing Loss and Tinnitus
Rapidly progressive bilateral sensorineural hearing loss is defined as a shift of 15 dB or more at any frequency or 10 dB or more at two or more consecutive frequencies, or a significant change in discrimination score occurring within three months of each other. Tinnitus is typically associated with sensorineural hearing loss and is more common in women aged 30 to 60 years. If the patient responds positively to steroid medication, the hearing loss is diagnosed as immune-mediated.
Ototoxicity
Ototoxic medicines and chemicals may impair the auditory system, resulting in functional damage to cochlear hair cells. As a result, they may cause tinnitus or hearing loss. The symptoms appear during or after the cessation of use. Audiometry reveals neurosensory bilateral hearing loss, symmetric or asymmetric, with one ear affected later. Currently, more than 150 medicines are recognized as ototoxic. The most commonly used medications include aminoglycosides (irreversible), vancomycin (irreversible), macrolide antibiotics (reversible), platinum-based anticancer medicines (irreversible), loop diuretics (reversible), and quinine. Salicylate is commonly used as a pain reliever, which is interesting. When used in high amounts, it may cause mild to moderate hearing loss. Hearing loss is often bilateral and symmetric, and it is coupled with tinnitus; both the hearing loss and the tinnitus normally resolve within 24 to 72 hours of stopping the medicine.
Auditory Neuropathy Spectrum Disorder
Auditory neuropathy spectrum disorder (ANSD) is a retro-cochlear hearing condition characterized by normal functioning outer hair cells (as evidenced by a normal otoacoustic emission response) or cochlear microphonics, absent middle ear muscle reflexes, and an absent/abnormal auditory brainstem response. Clinically, ANSD is characterized by poor speech recognition, which is heavily influenced by background noise and does not correspond to pure tone thresholds. Other symptoms include headaches, tremors, balance issues, vertigo, and weariness.
Tinnitus and the vestibular system
Vestibular Migraine and Tinnitus
Tinnitus occurs in around 46% to 68% of instances of vestibular migraine. The diagnosis of vestibular migraine is based on the presence of recurring vestibular symptoms that occur before, during, or after migraine. In the absence of another diagnosis, symptoms include headache, visual aura, photophobia, and phonophobia in at least half of the episodes. Vestibular migraine bouts can last anywhere from a few minutes to days. Fluctuating hearing loss and auditory fullness may also be present, as evidenced by a modest sensorineural hearing loss on the audiogram. Vestibular migraines can occur at any age, but they are more common in middle-aged women. Stress, a lack of sleep, dehydration, specific meals, or physical exercise can all provoke episodes. Among women of reproductive age, assaults coincide with the menstrual cycle.
Benign Paroxysmal Positional Vertigo and Tinnitus
Benign paroxysmal positional vertigo (BPPV) is a common peripheral vestibular condition of the semicircular canals that is triggered by certain head movements, resulting in recurring, brief vertigo attacks. Most cases are caused by abnormally displaced otoconia into the semicircular canals, resulting in a mistaken impression of head rotation and nystagmus. Provocative maneuvers are used to determine the diagnosis, which results in a specific pattern of nystagmus in the plane of the afflicted canal. BPPV is often a self-limiting illness, but it can impede with everyday activities and increase the risk of falls in senior people. Tinnitus is linked to the onset of positional vertigo in around 19% of people with BPPV. Tinnitus is intermittent, mildly strong, typically unilateral, and located in the same ear as the BPPV; it ceases or reduces immediately or shortly after the repositioning operation.







